Pregnancy-related deaths are a pressing public health issue that highlights significant gaps in healthcare access and quality for mothers in the United States. Alarmingly, over 80% of these deaths are deemed preventable, yet the nation continues to lead high-income countries in maternal mortality rates. A recent study indicates that this trend is not only persistent but worsening, revealing stark racial disparities in maternal health outcomes. For instance, American Indian and Alaska Native women face nearly four times the mortality risk compared to their white counterparts. The urgent need for improved prenatal and postpartum care cannot be overstated, as it is crucial for addressing preventable deaths during pregnancy and enhancing overall maternal health.
Maternal death during pregnancy and the postpartum period remains an acute concern within America’s healthcare landscape. The term ‘maternal mortality’ encompasses fatalities arising from complications during or after childbirth, with a significant number attributed to insufficient medical intervention. Recent findings shed light on alarming trends, showcasing disparities among different racial and ethnic groups when it comes to healthcare access for mothers. Continuing fatalities from preventable causes underline the critical importance of comprehensive postpartum care and early intervention strategies. As we delve deeper into this subject, it becomes clear that addressing these complexities is vital to reversing the tide of increasing maternal fatalities.
Understanding Pregnancy-Related Deaths in the U.S.
In recent years, the alarming rise in pregnancy-related deaths in the United States has brought maternal mortality into sharp focus. According to recent studies, more than 80 percent of these deaths are preventable, highlighting a failure in the healthcare system to ensure safe childbirth. This situation is particularly concerning given that the U.S. leads other high-income countries in maternal mortality rates, a stark indicator of the systemic issues within obstetric care. The statistics reveal a troubling trend, with the mortality rate increasing from 25.3 to 32.6 deaths per 100,000 live births between 2018 and 2022. This upward trajectory raises questions about the underlying causes and necessitates an urgent revisiting of healthcare policies.
One of the core reasons behind this high maternal mortality rate is the inadequate access to optimal prenatal and postpartum care. Many women, especially those from marginalized communities, face barriers that prevent them from receiving timely medical intervention during their pregnancies. This is exacerbated by socioeconomic factors and systemic racial disparities that create inequitable access to maternal healthcare. Understanding the demographics and statistics—such as the significantly higher mortality rate among American Indian and Alaska Native women—should compel healthcare policymakers to implement strategies that focus on reducing these disparities and improving healthcare access for all mothers.
Racial Disparities in Maternal Health
Racial disparities in maternal health are a critical factor contributing to pregnancy-related mortality in the U.S. Research indicates that minority women, particularly non-Hispanic Black and Indigenous women, experience substantially higher rates of maternal death compared to their white counterparts. For instance, in the recent study, the mortality rate for American Indian and Alaska Native women was an alarming 106.3 per 100,000 live births, indicating a systemic inequity that cannot be ignored. These disparities are not merely statistics but represent real lives deeply affected by limitations in healthcare access, quality of services, and social determinants such as income and education.
Efforts to address these disparities must be holistic and multifaceted. Solutions include implementing targeted public health strategies that focus on culturally competent care and community engagement. Additionally, breaking down existing biases within healthcare systems is crucial to ensure that all women receive equitable treatment throughout their pregnancies. Enhancing maternal health education, improving healthcare access, and expanding postpartum care resources are essential steps toward creating an equitable healthcare environment that can substantially reduce racial disparities in maternal health outcomes.
The Importance of Postpartum Care
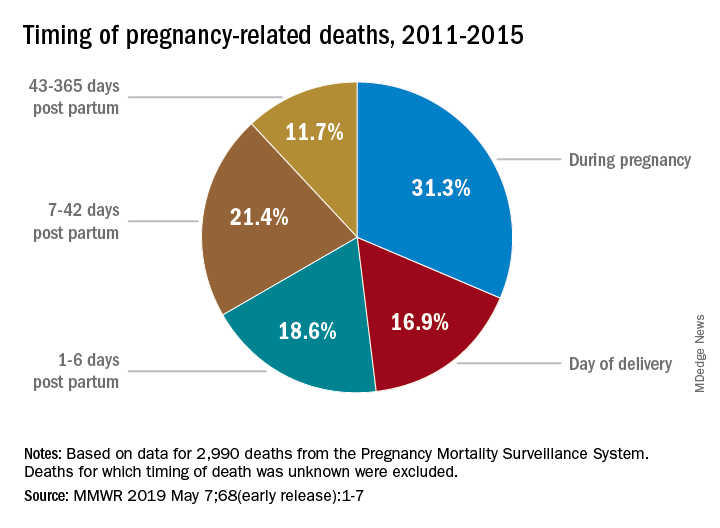
While prenatal care is often emphasized during pregnancy, postpartum care is critical for reducing pregnancy-related deaths. The recent study highlighted that nearly a third of maternal deaths occur between 42 days and one year after delivery, a period that is often overlooked in traditional maternal health models. As healthcare providers focus predominantly on the initial six-week postpartum period, many women may remain vulnerable to adverse health conditions that arise later. This oversight underscores the necessity to redefine the postpartum continuum, ensuring that maternal health care extends beyond the immediate post-delivery period.
Comprehensive postpartum care can help in managing chronic conditions that might develop during or after pregnancy, such as cardiovascular disease, which has emerged as a leading cause of maternal death. A proactive approach to postpartum care that includes regular check-ups, mental health support, and chronic disease management is essential for improving maternal health outcomes. By prioritizing extended care for new mothers, we can not only reduce the incidence of preventable deaths but also promote healthier families and communities.
Investment in Public Health Infrastructure
Building a robust public health infrastructure is paramount for addressing the rising rates of pregnancy-related deaths in the U.S. The stagnation in improvement and the upward trend in mortality rates signal a dire need for increased investment in maternal health programs. These investments should target various aspects, including healthcare access for mothers, the training of healthcare providers, and the enhancement of data tracking systems to better understand and respond to maternal mortality. The implementation of comprehensive public health strategies can create a more equitable health landscape, particularly for underserved populations.
Furthermore, funding should prioritize innovative solutions that address the quality of care during pregnancy and the postpartum period. This includes supporting community-based initiatives that aim to engage and educate mothers about their health rights and available resources. A comprehensive approach that encourages collaboration among healthcare providers, policymakers, and communities can foster sustainable improvements in maternal health, reduce preventable deaths during pregnancy, and ultimately lead to healthier generations.
Addressing Chronic Conditions in Pregnant Women
The increase in chronic conditions such as hypertension and cardiovascular disease among younger populations is a growing concern in maternal health. More women of reproductive age are being diagnosed with conditions that can complicate pregnancy and lead to severe outcomes. This shift towards younger individuals developing chronic diseases highlights the importance of pre-pregnancy health interventions. Screening for chronic conditions before and during pregnancy can aid in managing risks and improving health outcomes for mothers and their babies.
Integrating chronic disease management into prenatal care can help in addressing these emerging health issues among pregnant women. By establishing a preventive care approach, healthcare providers can better support women in maintaining their health and well-being during pregnancy. This focus on disease prevention not only helps in reducing pregnancy-related deaths but also contributes to a more informed and healthier population of mothers who can nurture their families effectively.
Policy Changes Needed to Improve Maternal Health
At the core of the rising pregnancy-related deaths is the need for substantial policy changes that align with the realities of maternal health in the U.S. Current policies often reflect a fragmented approach to maternal care, resulting in varying outcomes across states. For instance, California exhibits significantly lower pregnancy-related death rates, suggesting that targeted state policies can have meaningful impacts on maternal health. By examining what works in lower-mortality states, policymakers can adopt best practices that ensure all women receive adequate care regardless of their location.
Moreover, a comprehensive policy overhaul is necessary to address the social determinants of health that disproportionately affect marginalized communities. To achieve equitable health outcomes, policies must focus on improving healthcare access, providing adequate postpartum care, and reducing systemic biases in treatment. As stakeholders advocate for these changes, it is crucial to emphasize the importance of continuous investment in maternal health and public health infrastructure to sustain improvements over time.
Leveraging Community Resources for Maternal Support
Community resources play a pivotal role in improving maternal health outcomes and addressing the rise in pregnancy-related deaths. Local organizations and support networks can offer crucial services that extend beyond clinical care, such as educational programs, mental health support, and peer mentorship for new mothers. By leveraging these community-based resources, pregnant women can access vital information and support systems that help them navigate the complexities of motherhood and healthcare.
Engaging communities in maternal health initiatives also fosters a sense of belonging and support among expecting mothers. Programs that encourage community involvement not only provide peer support but also build awareness about the systemic barriers that contribute to maternal mortality. By cultivating stronger community ties and support networks, we can enhance the overall health of mothers and their infants, ultimately reducing preventable deaths during pregnancy.
The Role of Healthcare Providers in Maternal Health
Healthcare providers are the frontline defenders against rising maternal mortality rates in the U.S. Their role extends beyond traditional medical care to include advocating for women’s rights and health outcomes. Training programs that emphasize cultural competency, bias recognition, and effective communication can empower providers to better understand and serve diverse populations. By enhancing the training of healthcare professionals, we can create a more responsive healthcare system that recognizes the unique needs of each patient.
Furthermore, fostering collaborative relationships among healthcare providers across different specialties can improve the quality of care during pregnancy. Coordination between obstetricians, primary care physicians, and mental health professionals is essential for comprehensive maternal care. By working together, healthcare providers can address both physical and mental health challenges, providing integrated support that significantly lowers the risk of pregnancy-related complications. This synchronized approach not only bolsters maternal health but also promotes better outcomes for newborns.
Educating Women on Maternal Health Issues
Education is a powerful tool in combating the rising rates of pregnancy-related deaths by empowering women with knowledge about their health. Informative programs that teach women about the signs and symptoms of pregnancy complications can lead to earlier interventions and better outcomes. This education should include information on managing chronic conditions, understanding postpartum care, and recognizing the importance of follow-up appointments after birth. by equipping women with this knowledge, we can foster a generation of more informed mothers.
Additionally, addressing misconceptions about maternal health through public campaigns can improve overall awareness and encourage women to seek help when needed. Public health initiatives that focus on informed decision-making, access to healthcare services, and resources can make a substantial difference in maternal outcomes. In a country where pregnancy-related deaths are largely preventable, equipping women with the right information and support can drastically change the landscape of maternity care and health.
Frequently Asked Questions
What contributes to the rising rates of pregnancy-related deaths in the U.S.?
The rising rates of pregnancy-related deaths in the U.S. can be attributed to several factors including a fragmented healthcare system, inequitable access to maternal care, and persistent racial disparities in maternal health outcomes. Solutions need to tackle these systemic issues to reduce preventable deaths during pregnancy.
How significant are racial disparities in maternal mortality in the U.S.?
Racial disparities in maternal mortality are significant in the U.S., with American Indian and Alaska Native women facing the highest rates, followed by non-Hispanic Black women. These disparities point to systemic bias and inequities in healthcare access, which must be addressed to reduce pregnancy-related deaths.
Why are postpartum care and tracking late maternal deaths important for reducing pregnancy-related deaths?
Postpartum care is crucial because nearly a third of pregnancy-related deaths occur between 42 days to one year after childbirth. Addressing this period as part of ongoing maternal care can significantly reduce pregnancy-related mortality by ensuring women receive comprehensive health support beyond the early postpartum weeks.
What role does healthcare access play in pregnancy-related deaths?
Healthcare access is a critical factor in maternal health, with many preventable deaths occurring due to disparities in access to quality prenatal and postpartum care. Improving healthcare access for mothers is essential to lowering rates of preventable deaths during pregnancy.
How has the COVID-19 pandemic influenced pregnancy-related deaths?
The COVID-19 pandemic has been linked to increased rates of pregnancy-related deaths, particularly noted in 2021. Challenges associated with the pandemic, including strained healthcare resources, likely exacerbated existing maternal health issues, contributing to rising mortality rates.
What can be done to lower the rates of pregnancy-related deaths?
To lower pregnancy-related deaths, it is essential to invest in public health infrastructure, improve quality of care during pregnancy and postpartum, and address state-level policy disparities. By implementing innovative healthcare solutions and prioritizing maternal health, we can significantly reduce preventable deaths.
| Key Points | Details |
|---|---|
| U.S. Maternal Mortality Rates | The U.S. has the highest maternal mortality rate among high-income countries, with rates rising from 25.3 deaths in 2018 to 32.6 deaths per 100,000 live births in 2022. |
| Preventability | Over 80% of pregnancy-related deaths in the U.S. are preventable, indicating a critical need for improved healthcare systems. |
| Racial Disparities | American Indian and Alaska Native women face the highest mortality rates (106.3 per 100,000), significantly higher than white (27.6) and Black women (76.9). |
| Leading Causes of Death | Cardiovascular disease has become the leading cause of pregnancy-related death, now accounting for over 20% of these fatalities. |
| Postpartum Care | Late maternal deaths (between 42 days and one year after pregnancy) represent nearly a third of total maternal deaths, stressing the importance of extended postpartum care. |
| Investment in Health Infrastructure | There is a pressing need for investment in public health infrastructure to address rising pregnancy-related deaths and improve healthcare quality during and after pregnancy. |
Summary
Pregnancy-related deaths in the United States are a growing concern, as the country leads high-income nations in maternal mortality. Recent studies have revealed alarming trends, including a significant rise in preventable deaths between 2018 and 2022, particularly among marginalized racial groups. The findings highlight the urgent need for reform in the healthcare system to provide better prenatal and postpartum care, ultimately aiming to reduce the mortality rate and address the stark inequalities present in maternal healthcare.