AI for predicting brain cancer relapse represents a groundbreaking advancement in cancer care, particularly in pediatric patients facing gliomas. Recent studies highlight how artificial intelligence can outperform traditional methods by analyzing multiple brain scans over time to assess the risk of recurrence. This innovative approach could revolutionize glioma treatment, offering more personalized and precise care for young patients recovering from brain cancer. By integrating AI in medicine, healthcare providers aim to alleviate the stress of frequent imaging required to monitor potential cancer recurrence. Embracing these technological advances in radiation oncology not only enhances cancer recurrence prediction but also fosters hope for improved outcomes in children affected by brain tumors.
The use of artificial intelligence to forecast relapses in brain cancer, especially among children diagnosed with gliomas, is emerging as a key focus in modern medicine. This high-tech solution aligns with the growing field of cancer recurrence prediction, where sophisticated algorithms analyze patient data over time. As healthcare professionals increasingly incorporate AI into treatment protocols, the potential for improved strategies in radiation therapy becomes apparent. Novel approaches, such as those capable of deciphering patterns from longitudinal imaging, may lead to more effective interventions tailored to individual patient needs. Through continued innovation, we can aspire to transform the landscape of pediatric brain cancer care.
Advancements in AI for Predicting Brain Cancer Relapse
Recent advancements in artificial intelligence have ushered in a new era in the realm of pediatric brain cancer management, particularly concerning the prediction of cancer relapse. A groundbreaking study conducted by researchers at Mass General Brigham has unveiled a novel AI tool that significantly enhances the accuracy of predicting relapse risks in pediatric patients diagnosed with gliomas. Unlike traditional methods that rely on isolated scans, this AI model utilizes a technique called temporal learning, which examines multiple brain scans taken over time. This comprehensive approach not only aids in identifying which patients are at higher risk of experiencing a relapse but also alleviates the emotional and physical toll of frequent magnetic resonance imaging (MRI) sessions on children and their families. This innovative AI technology could redefine follow-up protocols in radiation oncology, leading to more personalized treatment plans tailored to individual patient needs.
Furthermore, the accuracy of the AI tool, which boasts an impressive prediction rate of 75-89 percent, represents a substantial leap over the previous benchmarks of about 50 percent for single-image evaluations. Researchers emphasize that early identification of at-risk patients may pave the way for timely interventions, reducing the frequency of invasive imaging procedures for those at lower risk. Relapses in pediatric glioma cases can be devastating, and thus, having reliable predictive tools could transform patient management and enhance overall survival rates. The insights gained from this study highlight the potential of AI to revolutionize oncology practices, offering a glimpse into a future where treatment strategies are increasingly driven by intelligent analytics.
The Role of Temporal Learning in Medical Imaging
Temporal learning has emerged as an innovative method in AI that is set to change the landscape of medical imaging significantly. In the context of brain cancer treatment, this technique allows researchers to achieve precision by analyzing sequences of images obtained at various time points rather than relying on single scans. By chronologically ordering a patient’s MRIs post-surgery, the AI can track subtle changes over time in the brain’s condition, associating these transformations with potential recurrence of gliomas. This revolutionary approach elevates the predictive accuracy of AI tools, providing clinicians with valuable foresight into patient outcomes. It empowers healthcare providers with enhanced tools necessary for timely decision-making in highly critical cases of pediatric brain cancer.
Moreover, the application of temporal learning is not limited to brain oncology alone; it has implications for a variety of medical fields where longitudinal imaging is crucial for patient monitoring. For instance, conditions such as cardiac disease and chronic illnesses could greatly benefit from similar AI-driven insights, propelling a wave of technological integration across healthcare sectors. The hopes of researchers at Mass General Brigham to validate these findings through comprehensive clinical trials highlight a commitment to transforming theoretical advancements into practical solutions that can tangibly improve patient care outcomes.
Cancer Recurrence Prediction Using AI in Pediatric Patients
The ability to accurately predict cancer recurrence is a pivotal aspect of managing pediatric brain tumors like gliomas. AI techniques, particularly those leveraging deep learning algorithms, are becoming increasingly popular in this predictive realm. By analyzing vast datasets, including thousands of MRI scans from previous patients, AI can learn to distinguish between benign changes in the brain and those that signal a potential relapse. This predictive capability not only supports timely interventions but also strategically informs discussions about adjuvant therapies—treatments given in addition to the primary therapy to maximize their effectiveness.
Incorporating AI for predicting brain cancer relapse represents a promising avenue for improving prognosis and enhancing the quality of life for young patients. The implementation of such sophisticated technology in radiation oncology could lead to tailored care approaches, as doctors might opt to intensify treatment for high-risk individuals while sparing low-risk patients from unnecessary procedures. This personalized medicine model could be the key to not only improving survival rates in pediatric glioma cases but also in minimizing the stress associated with cancer treatment for children and their families.
Impact of AI on Pediatric Glioma Treatment Outcomes
The integration of AI tools in the treatment of pediatric gliomas carries the potential to dramatically alter clinical outcomes. By refining the accuracy of relapse predictions, healthcare teams can formulate targeted treatment plans that align with individual risk assessments. For children who exemplify a higher likelihood of recurrence, preemptive measures could be taken, such as early intervention with supplemental therapies. This proactive approach emphasizes the necessity of evolving traditional protocols in radiation oncology to be more data-driven, ultimately leading to better patient outcomes.
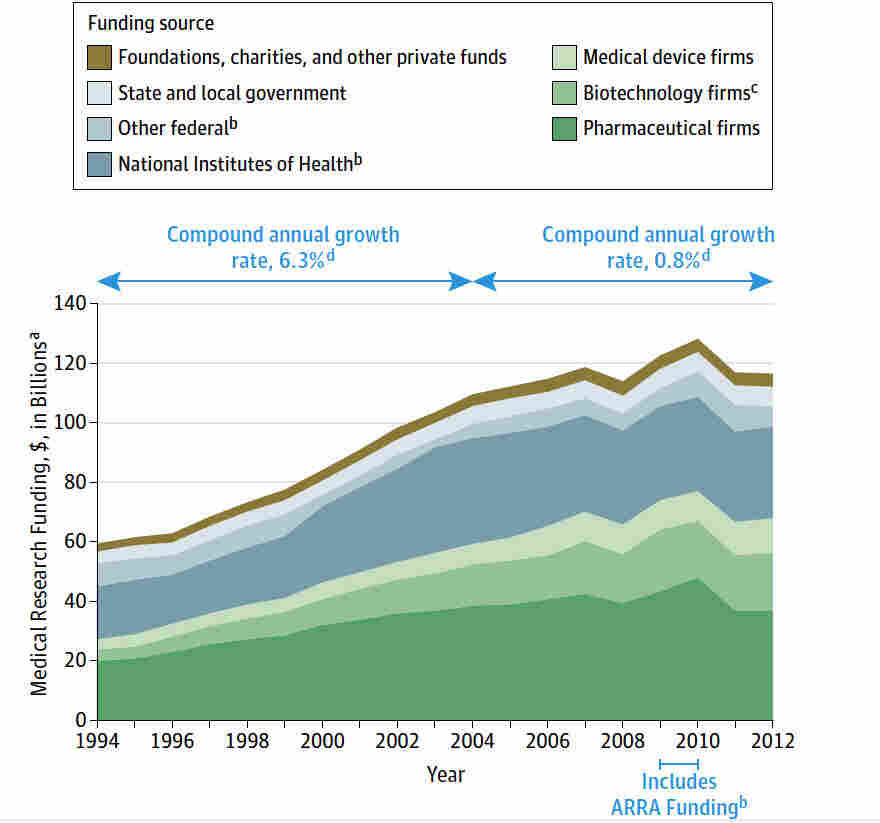
Moreover, the support garnered from institutions such as the National Institutes of Health underscores the broader implications of utilizing AI in oncology research. As advancements in AI continue to unfold, the implications for increasing the efficiency of care—coupled with improving survival rates—present a hopeful outlook for the future of pediatric cancer treatment. Enhanced AI tools are fueling a fundamental shift towards a more nuanced understanding of cancer behavior, allowing clinicians to anticipate needs rather than merely react, creating a more holistic treatment experience for patients.
Challenges and Considerations in AI Implementation
Despite the promising implications of AI in predicting brain cancer relapse, several challenges accompany its implementation in clinical practice. One significant concern remains the variability in imaging techniques and standards across different hospitals. For AI tools to function effectively, they require standardized data inputs to ensure accuracy and reliability. Researchers must engage in extensive validation processes across diverse clinical settings to establish trust in these predictive models. This will be essential for ensuring that the AI tool’s predictions consistently translate into tangible benefits for patients.
Additionally, ethical considerations surrounding AI’s role in patient care must be addressed. Safeguarding patient privacy and ensuring that sensitive medical data remain secure is paramount as healthcare systems increasingly incorporate AI technologies. Balancing innovation with ethical responsibility will be necessary to foster a climate where advancements in AI can be embraced by both medical professionals and patients alike. As the field of pediatric oncology navigates these complexities, the successful integration of AI could cement itself as a cornerstone of future treatment paradigms.
Future Directions in AI and Pediatric Brain Cancer Research
Looking forward, the future of pediatric brain cancer treatment is golden with the potential advancements AI can bring. Researchers are optimistic about building on the foundational knowledge gained from recent studies, envisioning a robust pipeline of AI-driven strategies that could refine the accuracy of cancer recurrence predictions even further. Continued exploration into machine learning algorithms can provide greater insights into the pathophysiology of gliomas, prompting revolutionary breakthroughs in treatment methods and patient care.
Clinical trials leveraging AI technologies are anticipated to be the next crucial step to validate and adapt these findings into everyday healthcare practices. By establishing a feedback loop where AI predictions can be evaluated and fine-tuned based on real-world outcomes, the medical community could witness a shift in cancer treatment paradigms, where AI not only assists in diagnosis but also in crafting precise, individualized treatment plans. The future is bright, and the prospect of a healthcare landscape enriched by AI in medicine promises to enhance the quality of life for many pediatric patients battling brain cancer.
The Importance of Multi-disciplinary Collaboration in Cancer Research
The success of AI in predicting cancer relapse hinges on collaboration among multiple disciplines within the healthcare ecosystem. For the advancements in AI to be relevant and applicable, diverse teams comprising radiologists, oncologists, data scientists, and AI specialists must collaborate closely. By pooling together their expertise, researchers can ensure that the systems they develop are not only technologically sound but also clinically relevant, refining their workflows to address the nuances of pediatric brain cancer treatment.
Moreover, cross-institutional collaboration fosters the sharing of critical data and resources that can significantly bolster research outcomes. As seen in the comprehensive studies conducted by Mass General Brigham in partnership with Boston Children’s Hospital and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, collaborative efforts can amplify the reach and impact of AI in medicine. Instituting a culture of teamwork in cancer research can catalyze breakthroughs that ultimately lead to more effective treatments and better survival rates for young patients facing neurological challenges.
Implications for Patient-Centered Care in Oncology
The utilization of AI tools in oncology not only enhances predictive capabilities but also profoundly influences patient-centered care paradigms. By accurately forecasting cancer relapse risks, clinicians can improve communication with patients and their families regarding prognosis and treatment strategies, ensuring that decisions reflect shared values and preferences. Heightened awareness of individual patient risks promotes a collaborative partnership between healthcare providers and families, thereby integrating the patient experience into the treatment process.
Furthermore, personalized care driven by AI insights can lead to significantly reduced anxiety for families by limiting unnecessary imaging and invasive procedures, ultimately fostering a more supportive healthcare environment. For pediatric patients, whose ability to comprehend their medical circumstances can be limited, the benefits of tailored communication and care can lead to improved adherence to treatment plans and overall satisfaction with care received. As AI continues to evolve within the medical field, the ripple effects on patient-centered care will undoubtedly reshape the future landscape of oncology.
The Future of AI in Medicine: Transforming Oncological Practices
The integration of AI into oncology is leading a transformative shift in healthcare practices, particularly in treatment and prevention strategies for diseases like pediatric brain cancer. The ongoing research illustrates a burgeoning recognition of the potential held by AI to refine diagnostic processes and enhance therapeutic outcomes. As tools become more sophisticated, the expectation is that they will provide not only predictive analytics but also actionable insights that can directly influence treatment protocols and resource allocation.
As we look toward a future enhanced by AI in medicine, it is paramount that ongoing education and training for healthcare professionals accompany these advancements. Familiarization with AI technologies will empower clinicians to leverage these tools effectively, ensuring optimal patient outcomes while keeping pace with the rapid evolution of medical knowledge. The hallmark of a truly integrated approach to cancer care will be a seamless synergy between human expertise and machine precision.
Frequently Asked Questions
How does AI improve predictions for pediatric brain cancer relapse compared to traditional methods?
AI tools enhance cancer recurrence prediction by analyzing multiple brain scans over time, significantly outperforming traditional single-scan methods. This approach allows for a more comprehensive understanding of subtle changes in pediatric patients with gliomas, leading to a prediction accuracy of 75-89% for relapse risk.
What role does temporal learning play in AI for predicting brain cancer relapse?
Temporal learning is a technique that enables AI models to assess changes in brain scans taken over time, rather than just examining single images. By sequencing MRIs chronologically, the AI can more effectively identify patterns and predict the relapse of pediatric brain tumors like gliomas.
What accuracy do AI tools provide in predicting brain cancer recurrence in children?
Research indicates that AI tools can predict the recurrence of pediatric brain cancer, specifically gliomas, with an accuracy of 75-89%, a substantial improvement over traditional methods that have an accuracy of around 50%.
Are there any ongoing studies related to AI in predicting brain cancer treatments and outcomes?
Yes, ongoing studies are focusing on validating the effectiveness of AI in predicting relapse risk among pediatric patients with gliomas. Researchers are exploring clinical trials to assess how AI-informed predictions can enhance treatment strategies and patient care.
How might AI influence the frequency of imaging required for pediatric brain cancer patients?
AI’s ability to accurately predict relapse risk could potentially reduce the frequency of imaging for low-risk pediatric brain cancer patients, alleviating stress and burden on families while ensuring high-risk patients receive timely interventions.
What implications do AI advancements have for the field of radiation oncology in treating pediatric brain tumors?
AI advancements are transforming radiation oncology by providing precise cancer recurrence predictions, enabling tailored treatment strategies for pediatric glioma patients and improving overall patient outcomes.
Is AI already being integrated into clinical practices for pediatric brain cancer?
While AI tools demonstrate promising predictions for brain cancer relapse, further validation and clinical trials are needed before widespread integration into routine clinical practices for pediatric oncology.
How can AI assist in the management of pediatric glioma patients post-surgery?
AI can aid in managing pediatric glioma patients by predicting the likelihood of cancer recurrence with enhanced accuracy through analysis of imaging over time, thus informing follow-up care and treatment modifications.
What future developments can we expect in AI applications for brain cancer research?
Future developments may include the broader application of AI models for various cancers, enhanced monitoring of treatment responses, and personalized therapy plans based on patient-specific imaging data.
What is the significance of using large datasets in training AI for cancer prediction?
Utilizing large datasets, such as the nearly 4,000 MR scans collected from pediatric patients, allows AI models to learn effectively, improving prediction accuracy and generalizability across diverse patient populations.
| Key Point | Details |
|---|---|
| AI Tool for Predicting Relapse | An AI tool predicts the risk of relapse in pediatric glioma patients more accurately than traditional methods. |
| Study Background | Conducted by researchers at Mass General Brigham and Boston Children’s Hospital using nearly 4,000 MR scans from 715 patients. |
| Temporal Learning Technique | This method uses multiple scans over time, allowing the AI to recognize changes and predict recurrence effectively. |
| Prediction Accuracy | The model predicted glioma recurrence with 75-89% accuracy, significantly better than the 50% accuracy of single-image predictions. |
| Future Implications | Further validation needed before clinical application; potential to improve patient care and treatment regimens. |
Summary
AI for predicting brain cancer relapse represents a significant advancement in pediatric oncology. This research demonstrates how artificial intelligence can enhance prediction accuracy for glioma recurrences by analyzing multiple MR scans over time. By utilizing temporal learning techniques, healthcare providers can better identify which patients are at higher risk of relapse, potentially transforming follow-up care and treatment strategies for pediatric patients. As AI continues to evolve in this field, it holds the promise of improving the quality of life for young cancer patients and their families.